Understanding Trauma Types
PTSD and CPTSD–From What Happened to What Comes Next
Here’s something I’d wish someone had told me years ago: your trauma doesn’t need to look a certain way to be valid.
For a long time, I minimized my own experiences because they didn’t fit the narrative I thought trauma required. No natural disaster. No combat zone. Just a childhood where the ground never felt stable, relationships that left invisible (and visible) bruises, and years of telling myself it “wasn’t that bad.”
Sound familiar? Let’s unpack what trauma actually looks like—and what it can become.
Big “T” and Little “t” Trauma
Researchers distinguish between two categories of trauma—not to rank suffering, but to understand how different experiences affect our minds (Cleveland Clinic, 2023).
Big “T” trauma includes events most people would find universally overwhelming: natural disasters, violent attacks, sexual assault, physical abuse, or military combat.
Little “t” trauma is trickier to recognize because it’s deeply personal. What devastates one person might barely register for another. Think: bullying, divorce, sudden relocation, financial stress, or the chronic invalidation of growing up in a home where your feelings didn’t matter.
Both types can fundamentally change how your brain processes safety, trust, and connection. And when trauma—especially repeated trauma—goes unaddressed, it can develop into something more persistent. Your Adverse Childhood Experiences (ACEs) score can be a good indicator or trauma.
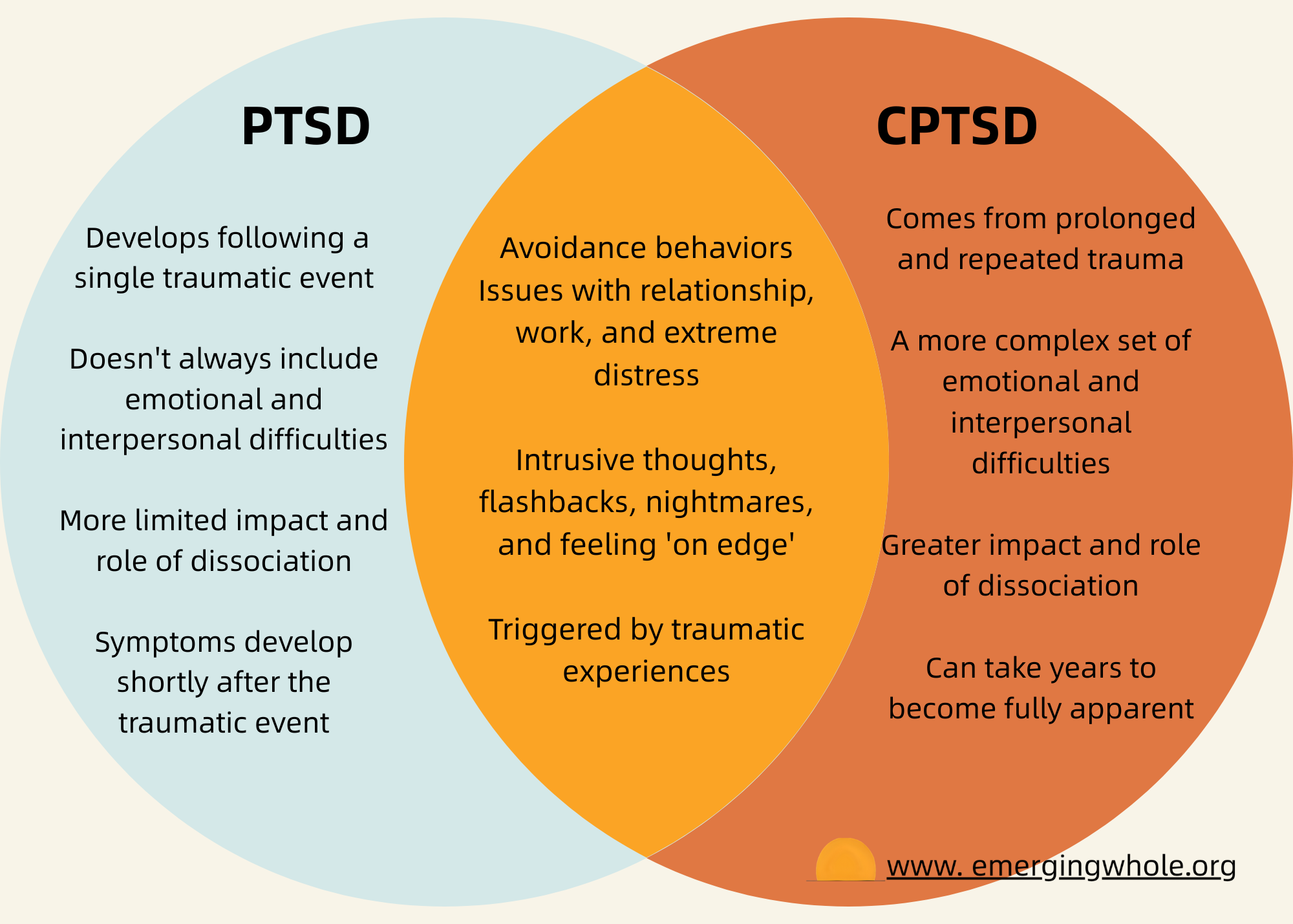
When Trauma Becomes PTSD
Post-traumatic stress disorder (PTSD) develops when your nervous system gets stuck in survival mode. Instead of processing the traumatic event and filing it away as “past,” your brain keeps sounding the alarm as if the danger is still happening (American Addiction Centers, 2025).
Common symptoms include:
• Re-experiencing the trauma through flashbacks, nightmares, or intrusive memories
• Avoidance of places, people, or situations that trigger memories
• Negative changes in mood and thinking—feeling detached, distrustful, or numb
• Heightened arousal—being easily startled, having trouble sleeping, feeling on edge
Complex PTSD: When Trauma Was Ongoing
Complex PTSD (CPTSD) develops from prolonged, repeated trauma—especially when escape felt impossible. This includes long-term childhood abuse or neglect, ongoing domestic violence, or being trapped in exploitative situations (Cleveland Clinic, 2023).
People with CPTSD experience PTSD symptoms plus additional challenges: difficulty regulating emotions, a fractured sense of identity, feeling permanently damaged or “different,” and struggling to maintain relationships. You might also experience emotional flashbacks—intense waves of fear, shame, or despair that flood you without a clear memory attached (Mind, 2021).
CPTSD is more likely to develop when trauma happened in childhood, lasted a long time, involved someone you trusted, or when multiple traumas compounded over time.
How Different Traumas Connect
Childhood and parental trauma is particularly impactful because it shapes your developing brain. When caregivers—the people meant to keep you safe—are the source of harm, it affects your fundamental sense of self-worth and ability to trust. This type of trauma frequently leads to CPTSD.
Sexual trauma can result from a single event or ongoing abuse. Both can lead to PTSD, but prolonged sexual abuse—especially in childhood—often results in CPTSD with additional complications around body image, intimacy, and self-blame.
Relationship trauma from manipulation, gaslighting, or emotional abuse can be harder to recognize but equally damaging. When someone systematically undermines your reality, it erodes your sense of self and can contribute to both PTSD and CPTSD symptoms.
The Connection to Substance Use and Maladaptive Behaviors
There’s a strong connection between trauma and turning to substances or other maladaptive behaviors for relief. Research shows that 25% to 49% of people with PTSD also struggle with substance use (Gottlich, 2025). It makes sense—when you’re drowning in anxiety, flashbacks, or emotional pain, anything that provides temporary escape feels like survival.
But substances that numb the pain temporarily often make trauma symptoms worse over time. They interfere with emotional regulation, disrupt relationships, and prevent the real healing work from happening. If this resonates with you, know that addressing both the trauma and the maladaptive coping isn’t optional—it’s necessary for genuine recovery.
The Other Side: Post-Traumatic Growth
Here’s what keeps me going: trauma doesn’t have to be the end of your story. Researchers have documented something called post-traumatic growth (PTG)—positive transformation that can emerge from struggling with highly challenging circumstances (Jean-Berluche, 2024).
PTG can include:
• Greater personal strength and self-understanding
• Deeper, more meaningful relationships
• A new appreciation for life
• Recognition of new possibilities
• Spiritual or existential growth
This doesn’t mean trauma is “good” or necessary for growth. It means that even in our darkest chapters, transformation is possible. Resilience—the ability to adapt and bounce back—is the key factor in post-traumatic growth.
Practical Tools for Moving Forward
Healing from trauma isn’t about pretending it didn’t happen. It’s about building new pathways forward.
Seek professional support. Trauma-informed therapies like Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) have strong evidence for treating PTSD and CPTSD. A trained professional can help you process memories safely.
Practice grounding techniques. When flashbacks hit, anchor yourself in the present. Try the 5-4-3-2-1 method: name five things you see, four you can touch, three you hear, two you smell, one you taste.
Develop emotional regulation skills. Learn to identify and name your emotions. Practice self-compassion—talk to yourself the way you’d talk to a friend who survived what you survived.
Build a support network. You don’t have to share your whole story with everyone. But finding even one person who believes you—or connecting with others who understand—can change everything.
Avoid substances as coping mechanisms. If you’re already using substances or other behaviors to manage symptoms, consider seeking support that addresses both the trauma and the coping pattern.
Recovery isn’t linear. Some days you’ll feel like you’ve made tremendous progress; others, you’ll wonder if you’ve moved at all. Both are part of the journey.
Your trauma is valid—whatever form it takes. Your healing matters. And your capacity for growth? It’s greater than you know.
References
American Addiction Centers. (2025, April 30). Post-traumatic stress disorder (PTSD) and addiction: Signs, symptoms, and treatment. https://americanaddictioncenters.org/co-occurring-disorders/trauma-stressor-related-disorders/ptsd-and-addiction
Cleveland Clinic. (2023, April 5). CPTSD (Complex PTSD). Cleveland Clinic Health Library. https://my.clevelandclinic.org/health/diseases/24881-cptsd-complex-ptsd
Gottlich, B. (2025, January 1). What is complex PTSD and how does it relate to addiction? Psychiatry NYC. https://www.psychiatrynyc.com/blog/what-is-complex-ptsd-and-how-does-it-relate-to-addiction/
Jean-Berluche, D. (2024). Intersecting paths: Substance use disorder recovery and post-traumatic growth. Journal of Substance Use, 30(3), 373–376. https://doi.org/10.1080/14659891.2024.2335477
Mind. (2021, January). Complex PTSD. https://www.mind.org.uk/information-support/types-of-mental-health-problems/post-traumatic-stress-disorder-ptsd-and-complex-ptsd/complex-ptsd/
Same Struggle, Different Source: Why CPTSD and BPD Get Confused
If you’ve been diagnosed with borderline personality disorder (BPD) but it never quite fit—or you’ve bounced between diagnoses—you’re not alone. Complex PTSD is frequently misdiagnosed as BPD, even though CPTSD is actually the more common condition.
Why the confusion? On the surface, they look remarkably similar. Both involve emotional dysregulation, relationship struggles, and dissociation. Both can stem from childhood trauma. But dig deeper, and the differences matter—especially for treatment.
Where They Overlap
• Difficulty regulating emotions
• Unstable or troubled relationships
• Dissociation under stress
• Feelings of emptiness or numbness
• Can co-occur (you can have both)
The Key Differences
Cause: CPTSD is caused only by repeated, prolonged trauma—usually in childhood. BPD can be caused by trauma, genetics, or both. Research suggests up to 50% of people with BPD have close relatives with the disorder.
Self-identity: This is a major distinguisher. People with BPD struggle with knowing who they are at their core—their sense of self shifts constantly. People with CPTSD typically have a more stable sense of self, but it’s marked by shame, guilt, and feeling “permanently damaged.”
Relationship patterns: Both struggle with relationships, but differently. CPTSD leads to avoiding close relationships due to deep distrust. BPD leads to seeking close relationships but struggling to maintain them—often swinging between idealizing and devaluing people.
Emotional regulation: Here’s a key clinical distinction. People with CPTSD tend to over-regulate—they shut down, numb out, withdraw. People with BPD tend to under-regulate—emotions explode outward as anger, impulsivity, or self-harm.
Why Getting It Right Matters
Treatment looks different. BPD treatment focuses heavily on behavioral and social skills—learning to regulate emotions and maintain stable relationships. CPTSD treatment is more individualized and trauma-focused, often requiring careful pacing because constantly addressing trauma can be overwhelming.
If you’ve been treated for BPD but aren’t seeing progress—or the diagnosis never quite resonated—it may be worth exploring whether CPTSD is a better fit. A trauma-informed mental health professional can help you sort through the overlap and find the path forward that actually addresses what’s underneath.
The right diagnosis isn’t about labels—it’s about finding the treatment that actually helps you heal.